Interventional Oncology Treatment
Minimally Invasive Cancer Treatments in Oceanside & Escondido
Interventional Oncology is the non-surgical, minimally-invasive, targeted treatment of cancer using imaging guidance. This allows for effective treatment and quick recovery for patients with less risk of pain and injury that is seen with other treatment methods, like surgery and radiation. Often, the treatment methods can be used as in combination with chemotherapy, surgery and/or radiation, to strive for the best result for the patient. The cancers we typically treat include those both primary and metastatic in liver, kidney, lung, bone and soft tissues. Depending on the type and location of cancer, we strive to achieve long-term control of tumor, including cure for some tumors.
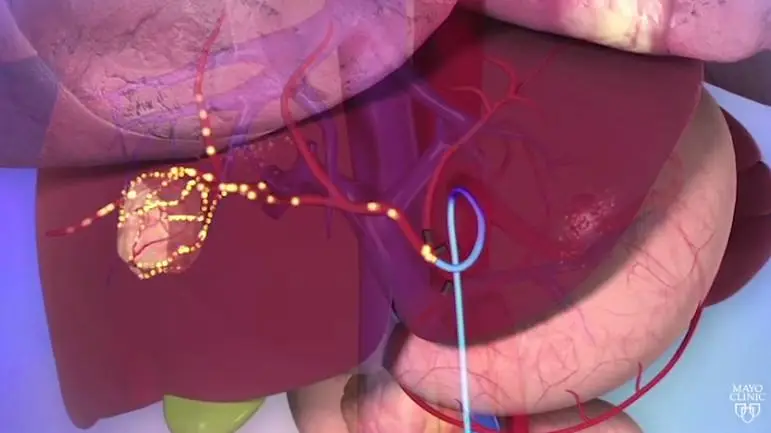
Transarterial radioembolization (TARE) or Y-90
Exclusively performed by trained vascular and interventional radiologists for treatment of liver cancer (HCC or hepatocellular cancer) or metastases by inserting a small catheter via the wrist or the groin. The incision is less than 3 mm. The catheter is then advanced into the small liver arteries supplying the tumor using X-ray or fluoroscopic guidance.
Millions of tiny particles, less than width of a strand of hair, containing radiation are then delivered to the blood supply of the tumor. The tumor will die after several weeks, but the normal liver remains unaffected.
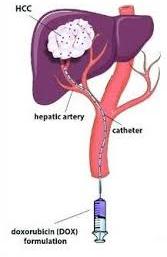
Transarterial chemoembolization (TACE)
Exclusively performed by trained vascular and interventional radiologists for treatment of liver cancer (HCC or hepatocellular cancer) or metastases by inserting a small catheter via the wrist or the groin.
The incision is less than 3 mm. The catheter is then advanced into the small liver arteries supplying the tumor using X-ray or fluoroscopic guidance. Millions of tiny particles, the size of a grain of sand and sometimes carrying chemotherapy, are delivered to tumor. These arteries are then blocked using these small particles.
This starves the cancer of the nutrients it receives from blood, and bathes tumor in high concentration, localized chemotherapy (if used) and the cancer dies. Patients with liver cancer confined only to liver or predominantly in liver with good liver function are candidates for this treatment.
After the procedure, patients can have 2-3 days of pain, fever or nausea, and tend to spend one night in the hospital after the procedure to ensure symptoms are controlled with medications. Patients will have follow-up CT or MRI every 2-3 months to ensure adequate treatment of cancer.
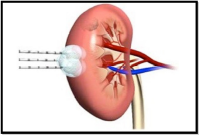
Ablation
Exclusively performed by trained vascular and interventional radiologists for treatment of cancer in the liver, kidney, lung, bone or soft tissues. Tiny needles placed directly through the skin into the tumor use special energy (microwave, radiofrequency ablation (RFA) or cryoablation) to freeze or heat the cancer so it dies, but normal tissue nearby isn’t harmed. CAT scan, ultrasound and/or X-ray is used to guide the needles to the exact spot of cancer.
This procedure sometimes requires general anesthesia, but it is an outpatient procedure, and you will be going home after 2-3 hours of recovery. There are small risks of bleeding and infection, and when treating in the lung, there’s a possibility of a couple days of a small chest tube if air develops around the lung. Patient’s typically have a quicker recovery from these procedures compared to surgery. After the procedure, patients will have follow-up CT or MRI every 2-3 months to ensure adequate treatment of cancer.